The case for thinking differently
[This blog was also published by the Independent Healthcare Providers Network]
Private healthcare finds itself at a crunch point.
Low (or no) growth across local and international markets, spiralling costs, falling medical insurance subscriptions and “intelligent consumerism” continue to challenge the sector. The basis for competition is also changing with the rise of digital health, more regulation, calls for increased transparency and new players entering the market. Moreover, managing across 3 payer groups (NHS, PMI and self-pay) and a philosophical shift away from fee-for service towards outcomes-based payment models is challenging clinical and management teams.
Setting winning strategies within this market complexity is not easy. The pressure to manage the urgent and not the important is great and endless planning is not a good substitute for proper strategy.
Old approaches to growth aren’t working. Doing more of the same cheaper or more efficiently isn’t going to deliver results over the longer-term. A new way of thinking and an ability to compete differently is required.
A unifying approach
Our “3P” approach” takes a broad, systems approach to thinking differently. Combining a better understanding of the population’s health, a wider look at the end to end pathway for long-term conditions and adopting people-participation in care design and delivery offers a compelling alternative way forward.
Our approach is contemporary (it’s where things are heading), it is evidence-based (there is precedent for these concepts), and it provides a more sustainable way of thinking about and developing winning strategies.
Population Health Management
Any business’ commercial strategy starts with a deep understanding of its customers. Unlike other industries, healthcare can be slow to understand its customers in a segmentedway and when it does, it tends to segment by disease or risk. People’s needs for healthcare are not defined by disease alone but by their holistic needs, their values and their preferences.
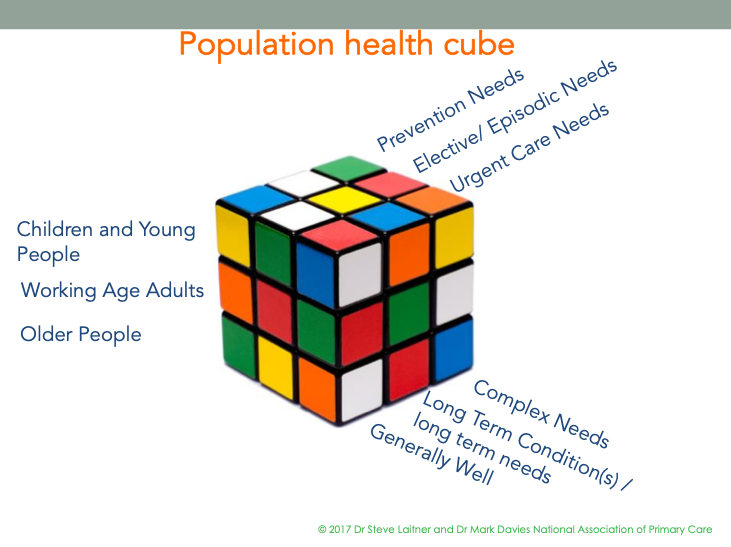
It can be helpful to think about segments of the population in a holistic way as described in the models below by one of the authors of this blog, in collaboration with the National Association of Primary Care (NAPC).
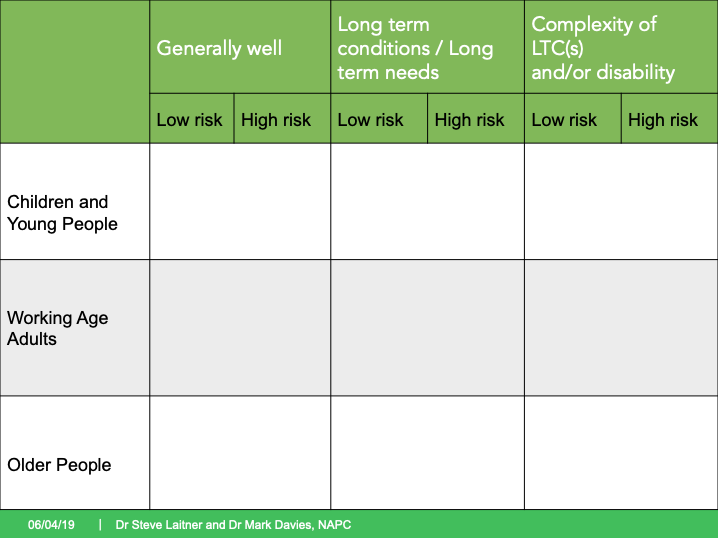
There are three major life-courses and three major levels of requirements for each life-course, each with its own particular needs, values and preferences. The various risk factors and diseases people have might define their clinical needs but not the physical, psychological and social support they might require.
For each area of this matrix people will have three different types of healthcare requirements as shown below:
The “Elective or Episodic” needs are likely to be for long term condition on-going management or for an “elective” operation or intervention, usually also in relation to a long-term condition.
Private healthcare has generally focussed on people’s episodic care needs, especially operations, without fully capturing the potential market for the on-going support for a person’s long-term condition(s), together with preventative strategies. It has also generally focussed on the working age adult population. When it comes to those who are “generally well” it tends to focus on the identification of risk factors through screening, wellness checks and tests, but not so much on the ongoing care and support people want and require in relation to prevention and wellness. Yet this ongoing care and support is what reduces their risk of future health problems and also, most importantly, improves their current quality of life.
Employing population health management techniques in this way may help providers look at their current market blind spots.
People Participation
The wisdom and insights that people with life-changing illness, injury and disability can bring is under-valued and traditional approaches to people/ patient engagement currently fail to have impact.
A new movement is happening in healthcare: “People Participation”.The NHS is leading on this with Patient Leaders and Patient Directors with lived experience in postwho are working way beyond being typical patient ‘reps’. They are shaping strategy with Executive teams based on their insights, skills and experience. They may bring in other Patient Partners to support their work on redesigning care.
David Gilbert, a leading Patient Director in the NHS and keynote speaker at the IHPN 2015 Annual Partnerships Summit, explains that People Participation values wisdom and insight of lived experience of illness, positions patients as allies for improvement and change, equalises power, endorses patients as system co-leaders and reframes the narrative in healthcare.
People Participation offers a more sustainable and consistent way of understanding what people, patients and carers really want. It involves patients as partners in the understanding of the current pathway, the issues to be addressed and in the design of the new pathway. Patients can also be involved in the delivery of care throughout the pathway…as a patient self-managing their long-term condition, as a carer caring and also as a peer, supporting other patients.
Private sector providers would be wise to start exploring the potential of “Patient Leaders” and “Patient Partners” to support their differentiation and growth.
Pathway
Any pathway of care can be seen from two perspectives – the provider perspective and the patient/carer perspective.
From the provider’s perspective, the end-end pathway is mostly unseen.
Private healthcare, particularly in the acute sector, typically funds, counts, and therefore manages the knee replacement, the endoscopy procedure, the gastric band or cardiac by-pass operation. But these patients are living for many years with osteoarthritis, reflux oesophagitis, obesity or angina, respectively. The sector may, therefore, only ‘see’ a small part of the whole patient pathway, missing out on seeing the totality of what patients, their families and carers go through in finding answers andseeking support with managing their long-term conditions.
Some might point to cancer care in the private sector as being different. The sector offers the one-stop shop of core diagnostics, surgical treatments, chemotherapy and radiotherapy elements of care along the pathway. Some providers do go further in offering complementary therapies, mental health support etc., but these are not a consistent feature across the sector. Moreover, they fall short of meeting all the ongoing needs (activities associated with the high burden of managing the disease for each patient, their families and carer), chiefly because these services are not reimbursed.
From the patients’ perspective, they are living with their condition 24/7. What they really want is support along the pathway, encouragement with shared-decision making i.e. ‘is this operation right for me at this time’, non-operative care, an operation if they need it, good aftercare and help with recovery and day to day living.
It is worth remembering that the only consistent thing in the end-to-end pathway is the patient. “Putting the patient at the heart of everything we do” is a familiar mantra, but often isn’t the case. One of the authors of this blog, in partnership with Wolff Olins (London) conducted a roundtable on exploring how service design thinking can make meeting people’s needs and preferences a practical outcome versus a value statement. Readers might find the outcomes of this session relevant here.
Touching and owning more of the pathway provides space for clearer differentiation of services offered by the sector. What follows is competitive advantage, new potential revenue streams and growth.
The Buyer Side
We recognise that an important part of this discussion is the need for buyer reform. While our intention here is not to offer a methodology for buyer reform, we can offer some observations to help move the debate on with buyers.
There will be different solutions for the 3 main buyer markets (NHS, self-pay and PMI). We’d suggest that the same principles presented above be applied to any buyer-reform, thinking differently about buyer segmentation across all 3 markets and being creative in sourcing solutions for these segments.
- The NHS might only be buying episodic interventions because that’s all that’s on offer. The NHS doesn’t have a great track record of commissioning or delivering services like health coaching, peer support, care planning support and long-term condition education. Private providers might uncover further opportunities for working with the NHS to deliver these services as part of a more comprehensive pathway of care. Moreover, in the future market place there will be a need for a different relationship between the NHS and private providers with the formation of Primary Care Networks, (the need for urgent ambulatory care) and more focus on mental health. These and other initiatives might stimulate a more on-going NHS/private relationship reflecting the on-going relationship with patients.
- PMIs will need to innovate their business models by using technology and better quality data to deliver more bespoke services to customers, including encouraging and supporting preventative behaviours
- Providers will also have to think differently if they want to leverage the growing self-pay market. This is the coal-face of going ‘beyond product towards experience’ and with it comes new opportunities to differentiate, build brands and customer loyalty. New incentives will follow.
How different and prepared do you want to be?
We recognise that this is brave, new stuff but we believe that our 3P approach presents a powerful, evidence-based way for private healthcare providers to think differently and reimagine how services can be delivered. The clinical and commercial case for doing so is compelling.
——————————- END —————————————–
Dr Steve Laitner, a senior clinical associate for Saffron Steer in multiple projects contributed to this blog. Steve is a practising General Practitioner with Public Health and clinical leadership background, who also works as a freelance Health Consultant, helping healthcare organisations to develop new models and systems of care.
Twitter: @SteveLaitner

